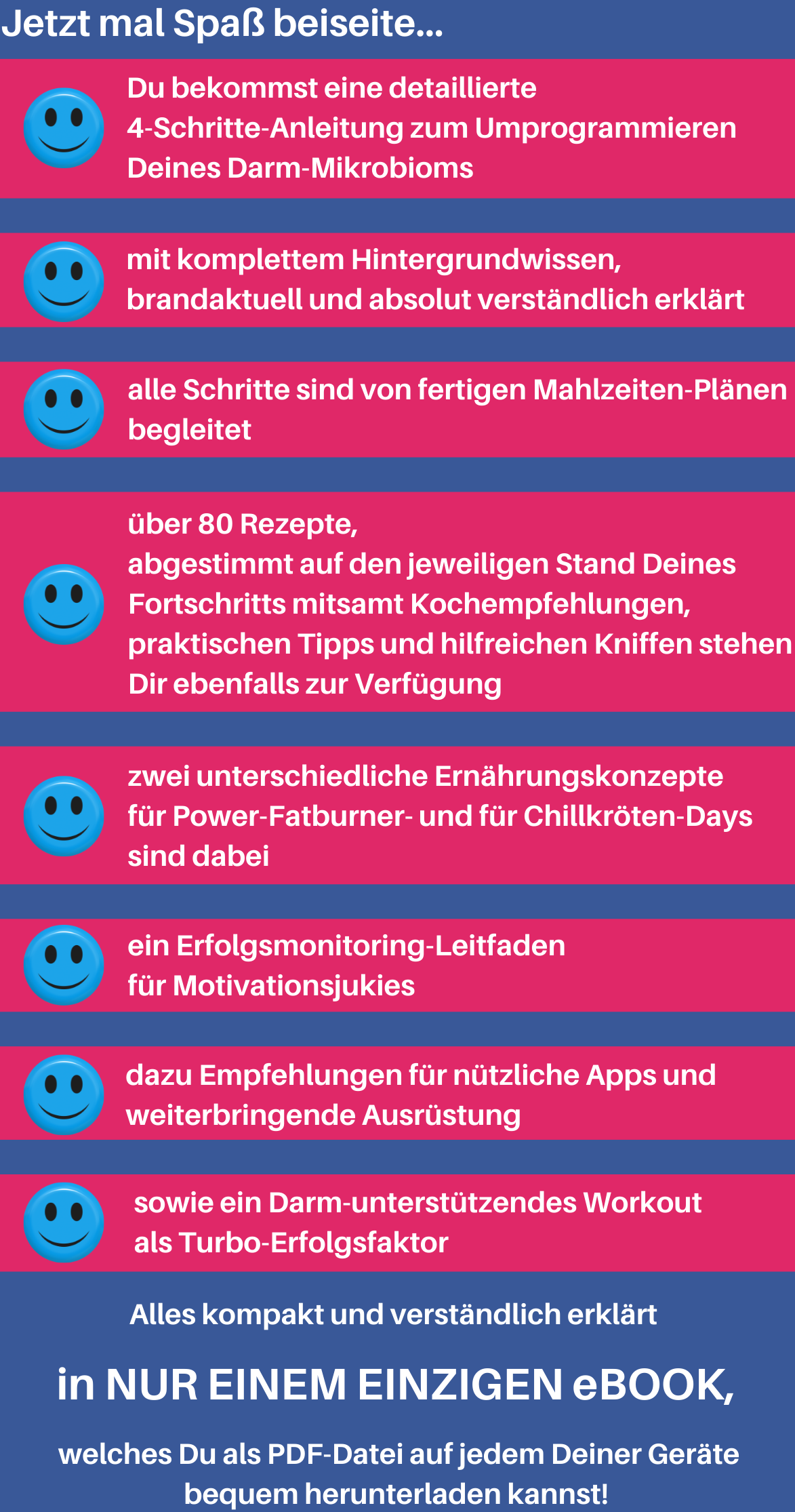
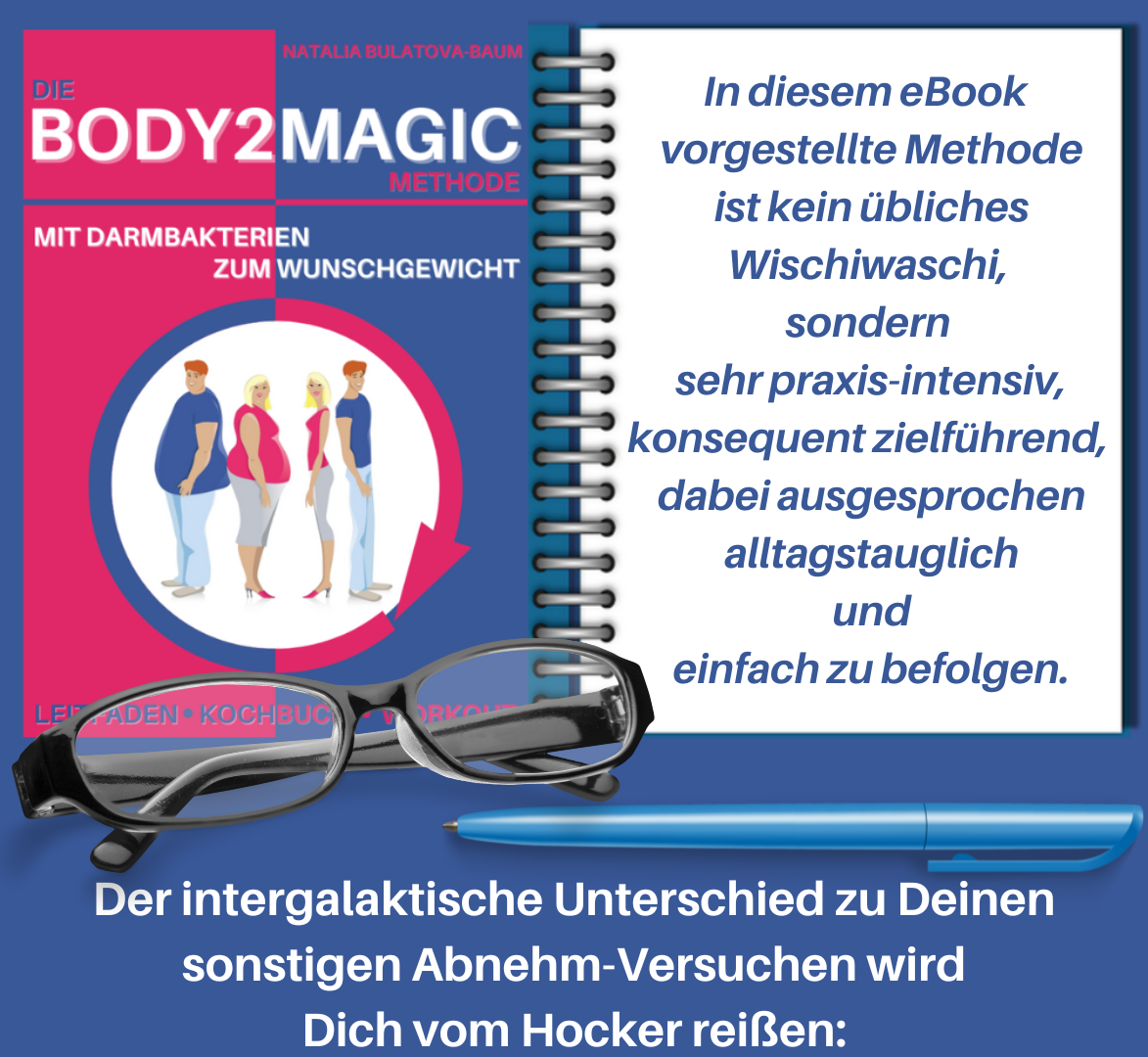
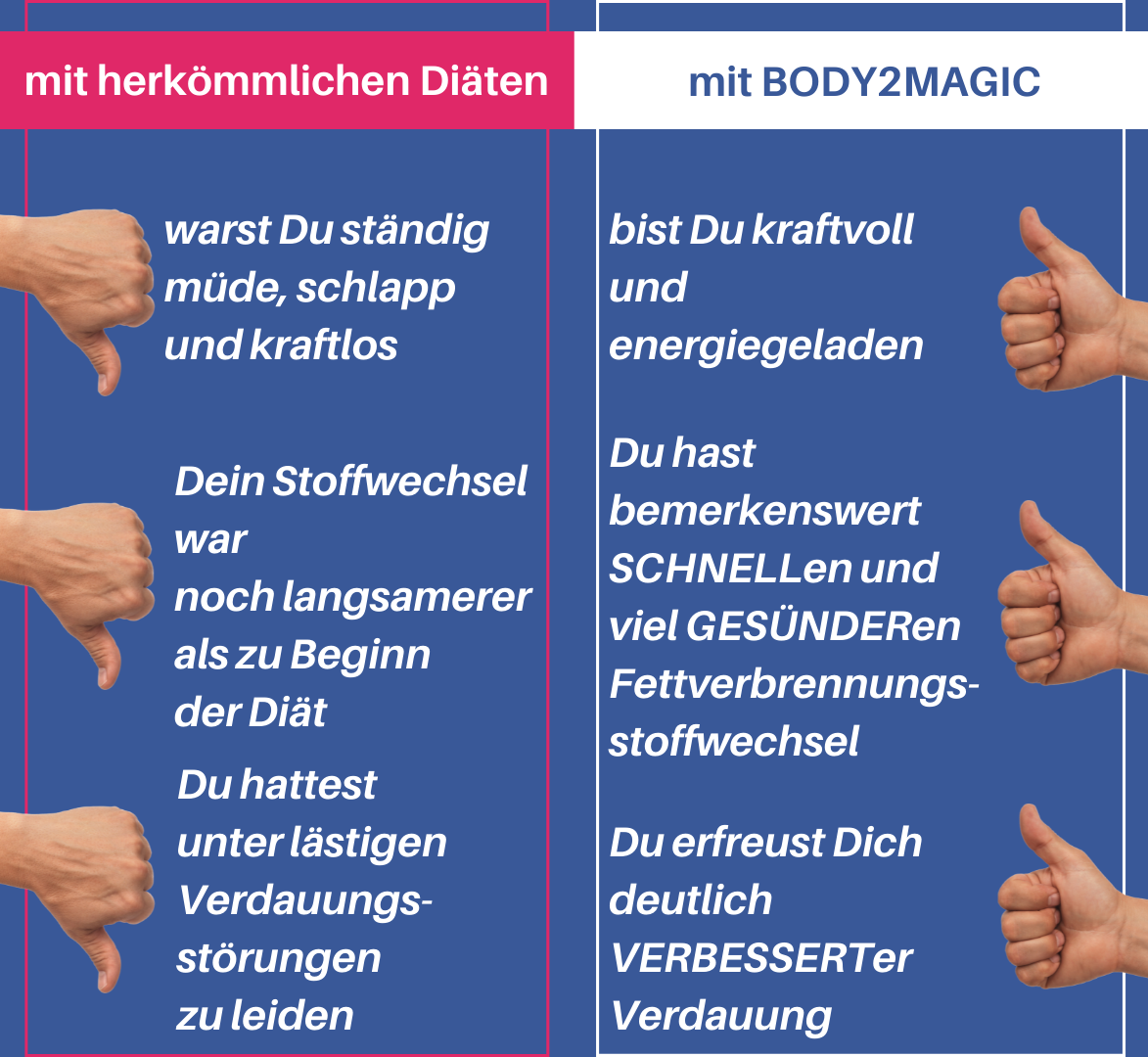
body2magic
die BODY2MAGIC-Methode



Aniwan S. et al: Antibiotic use and new-onset inflammatory bowel disease in Olmsted County, Minnesota: a population-based case-control study. Journal of Crohn's and Colitis (2018) 12(2): 137–144
Biragyn A. & Ferrucci L.: Gut dysbiosis: a potential link between increased cancer risk in ageing and inflammaging. Lancet Oncol (2018) 19(6): e295–e304
Blaser M.J: Fecal Microbiota Transplantation for Dysbiosis - Predictable Risks. New England Journal of Medicine (2019) Band 381, Ausgabe 21 vom 21. November 2919, Seiten 2064–2066 doi:10.1056/NEJMe1913807
Bosch Th.: Neue Bedrohungen für das Mikrobiom. Wiley Analytical Science (2021) doi: https://analyticalscience.wiley.com/do/10.1002/was.000600099
Bretin A. et al: Microbiota and metabolism: what’s new in 2018? American Journal of Physiology-Endocrinology and Metabolism (2018) 315(1): E1–E6
Candy D.C.A. et al: A synbioticcontaining amino-acid-based formula improves gut microbiota in non-IgE-mediated allergic infants. Pediatric Research (2018) Mar;83(3):677-686. doi: 10.1038/pr.2017.270
Chang C.J.: Next generation probiotics in disease amelioration. Journal of Food and Drug Analysis (2019) 27(3): 615–622
Chen X. et al: Alteration of the gut microbiota associated with childhood obesity by 16S rRNA gene sequencing. PeerJ 8, e8317 (2020)
Chong P.P. et al: The microbiome and irritable bowel syndrome — a review on the pathophysiology, current research and future therapy. Front Microbiol (2019) 10: 1136
Coelho L. P. et al: Similarity of the dog and human gut microbiomes in gene content and response to diet. Microbiome 6, 72 (2018)
Di Francesco A. et al: A time to fast. Science (2018) 362, 770–775
Eisele Y. et al: Fusobacterium nucleatum and Clinicopathologic Features of Colorectal Cancer: Results From the ColoCare Study. Clinical Colorectal Cancer (2021) Feb 27;S1533-0028(21)00021-9, doi: 10.1016/j.clcc.2021.02.007
Farzi A. et al: Gut Microbiota and the Neuroendocrine System. Neurotherapeutics. (2018); 15:5–22
Fehr K. et al: Breastmilk Feeding Practices Are Associated with the Co-Occurrence of Bacteria in Mothers’ Milk and the Infant Gut: the CHILD Cohort Study. Cell Host & Microbe (2020) 28(2), 285-297 doi: https://doi.org/10.1016/j.chom.2020.06.009
Finlay B. et al.: The hygiene hypothesis during a pandemic: consequences for the human microbiome. Proceedings of the National Academy of Sciences of the United States of America (2020) doi: https://doi.org/10.1073/pnas.2010217118
Floch M.H.: The role of prebiotics and probiotics in gastrointestinal disease. Gastroenterology Clinics of North America (2018) 47(1): 179–191
Frost F. et al: A structured weight loss program increases gut microbiota phylogenetic diversity and reduces levels of Collinsella in obese type 2 diabetics: a pilot study. PLoS ONE 14 (2019) e0219489
Gálvez E.J.C. et al: Distinct polysaccharide utilization determines interspecies competition between intestinal Prevotella spp. Cell Host & Microbe (2020) October doi: 10.1016/j.chrom.2020.09.012
GBD 2017 Diat Collaborators: Health effects of dietary risks in 195 countries, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet (2019) 393, 1958–1972
Guevara-Cruz M. et al: Improvement of lipoprotein profile and metabolic endotoxemia by a lifestyle intervention that modifies the gut microbiota in subjects with metabolic syndrome. Journal of the American Heart Association 8, e012401 (2019)
Hanson B.T. et al: Sulfoquinovose is a select nutrient of prominent becteria and sourch of hydrigen sulfide ib the human gut. ISME Journal (2021) doi: 10.1038/s41396-021-00968-0
Huang X. et al: Emerging trends and research foci in gastrointestinal microbiome. Journal of Translational Medicine (2019) 17(1): 67
Jia Yang & Jun Yu: The association of diet, gut microbiota and colorectal cancer: what we eat may imply what we get. Protein Cell (2018) 9(5): 474–487
Jefferson A. & Adolphus K. : The Effects of Intact Cereal Grain Fibers, Including Wheat Bran on the Gut Microbiota Composition of Healthy Adults: A Systematic Review. Frontiers in Nutrition (2019) 6, 33
Konturek P. et al: Intestinal microbiota — a vital “organ” with manifold functions. MMW Fortschritte der Medizin (2020) 162(Suppl 4):9-14
Kopf J.C. et al: Role of whole grains versus fruits and vegetables in reducing subclinical inflammation and promoting gastrointestinal health in individuals affected by overweight and obesity: a randomized controlled trial. Nutrition Journal 17, 72 (2018)
Kowalski K. & Mulak A.: Brain-Gut-Microbiota Axis in Alzheimer’s Disease. Journal of Neurogastroenterol and Motility (2019) 25(1):48–60. DOI:10.5056/jnm18087
Kunnackal J.G. et al: Dietary Alteration of the Gut Microbiome and Its Impact on Weight and Fat Mass: A Systematic Review and Meta-Analysis. Genes vol. 9,3 167. (2018) DOI:10.3390/genes9030167
Kushugulova A. et al: Metagenomic analysis of gut microbial communities from a Central Asian population. BMJ Open 8 (2018) e021682
Liu Z. et al: Gut microbiota mediates intermittent-fasting alleviation of diabetes-induced cognitive impairment. Nature Communications 11, 855 (2020)
Logsdon A.F. et al: Gut reactions: how the blood-brain barrier connects the microbiome and the brain. Experimental Biology and Medicine (Maywood) (2018) 243(2):159–165
Maier L. et al: Extensive impact of nonantibiotic drugs on human gut bacteria. Nature (2018) Marz 29; 555(7698): 623-628. doi: 10.1038/nature25979
Makki K. et al: The impact of dietary fiber on gut microbiota in host health and disease. Cell Host & Microbe (2018) 23(6):705–715
Mangiola F. et al: Gut microbiota and aging. European Review for Medical and Pharmacological Sciences (2018) 22 (21): 7404–7413
Martin R. et al: Searching for the bacterial effector: the example of the multi-skilled commensal bacterium Faecalibacterium prausnitzii. Front Microbiol (2018) 9: 346
McCoy K.D. & Thomson C.A..: The Impact of Maternal Microbes and Microbial Colonization in Early Life on Hematopoiesis. Journal of Immunology (2018) 200(8), 2519-2526 doi: https://www.jimmunol.org/content/200/8/2519
Mesnage R. et al: Changes in human gut microbiota composition are linked to the energy metabolic switch during 10 d of Buchinger fasting. Journal of Environmental Science and Health 8, e36 (2019)
Münch Ph.C. et al: Identification of Natural CRISPR Systems and Targets in the Human Microbiome. Cell Host & Microbe (2020) doi: 10.1016/j.chrom.2020.10.010
Noce A. et al: Impact of gut microbiota composition on onset and progression of chronic non-communicable diseases. Nutrients (2019) 11 (5)
Osadchiy V. et al: The Gut–Brain Axis and the Microbiome: Mechanisms and Clinical Implications. Clinical Gastroenterology & Hepatology (2019) Jan; 17(2):322–332
Ozkul C. et al: Structural changes in gut microbiome after Ramadan fasting: a pilot study. Beneficial Microbes 11 (2020) 227–233
Radke M.: Was macht die Muttermilch mit dem Mikrobiom?. Pädiatrie 33, 4 (2021). https://doi.org/10.1007/s15014-020-2463-1
Reitmeier S. et al: Arrhythmic gut microbiome signatures predict risk of Type 2 Diabetes. Cell Host & Microbe (2020) doi: 10.1016/j.chrom.2020.06.004
Rinninella E. et al: What is the healthy gut microbiota composition? A changing ecosystem across age, environment, diet, and diseases. Microorganisms (2019) 7(1)
Roager H. M. et al: Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut 68, 83–93 (2019)
Rühlemann M.Chr. et al: Genome-wide association study in 8,956 German individuals identifies influence of ABO histo-blood groups on gut microbiome. Nature Genetics (2021) 53, pages 147–155
Ryan D. et al: A high-resolution transcriptome map identifies small RNA regulation of metabolism in the gut microbe Bacteroides thetaiotaomicron. Nature Communications (2020) doi: 10.1038/s41467-020-17348-5
Sanders M.E. et al: Probiotics and prebiotics in intestinal health and disease: from biology to the clinic. Nature Reviews Gastroenterology & Hepatology (2019) 16(10): 605–616
Sanna S. et al: Causal relationships among the gut microbiome, short-chain fatty acids and metabolic diseases. Nature Genetics (2019) 51(4):600–605
Seelbinder B. et al: Antibiotics create a shift from mutualism to competition in human gut communities with a longer-lasting impact on fungi than bacteria. Microbiome (2020) 8, 133
Shin C. & Kim Y.K.: Autoimmunity in microbiome-mediated diseases and novel therapeutic approaches. Current Opinion in Pharmacology (2019) 49: 34–42
Sonnenburg J.L. & Sonnenburg E.D.: Vulnerability of the industrialized microbiota. Science (2019) 366 (6464), doi: https://doi.org/10.1126/science.aaw9255
Stockert K.: Allergie, Mikrobiom und weitere epigenetische Faktoren. Nature Public Health Emergency Collection (2020) Mar 25. German. doi: 10.1007/978-3-662-58140-7_4
Sun M.F. & Shen Y.Q.: Dysbiosis of gut microbiota and microbial metabolites in Parkinson‘s Disease. Ageing Research Reviews (2018) Aug; 45:53–61
Thingholm L.B. et al: Obese Individuals with and without Type 2 Diabetes Show Different Gut Microbial Functional Capacity and Composition. Cell host & microbe (2019) pages 252-264.e10
Valdes A.M. et al: Role of the gut microbiota in nutrition and health. BMJ (2018) 361: k2179
Velikonja A. et al: Alterations in gut microbiota composition and metabolic parameters after dietary intervention with barley beta glucans in patients with high risk for metabolic syndrome development. Anaerobe 55, 67–77 (2019)
Ventura M. et al: Health benefits conferred by the human gut microbiota during infancy. Microb Biotechnol (2019) 12(2): 243–248
Willyard C.: How gut microbes could drive brain disorders. Nature (2021) doi: 10.1038/d41586-020-01003-6
Zhang C. et al: Impact of a 3-months vegetarian diet on the gut microbiota and immune repertoire. Frontiers in Immunology 9, 908 (2018)
Zhao L. et al: Gut bacteria selectively promoted by dietary fibers alleviate type 2 diabetes. Science (2018) 359(6380):1151–1156
Zinöcker M.K. & Lindseth I.A.: The western diet—microbiome-host interaction and its role in metabolic disease. Nutrients (2018) 10(3):365
Zmora N. et al: You are what you eat: diet, health and the gut microbiota. Nature Reviews Gastroenterology & Hepatology (2019) 16(1): 35–56
Zou J, et al: Fiber-Mediated Nourishment of Gut Microbiota Protects against Diet-Induced Obesity by Restoring IL-22-Mediated Colonic Health. Cell Host Microbe (2018) Jan 10;23(1):41-53.e4. doi: 10.1016/j.chom.2017.11.003